Two recent studies conducted by researchers at The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) have provided significant insights into the effectiveness of the oral antiviral drug Paxlovid (also known as nirmatrelvir-ritonavir) on post-acute death and sequelae after COVID-19 infection, as well as its interaction with vaccination status. In the first study, researchers conducted the world’s first real-world analysis focusing on immunocompromised individuals, primarily revealing that Paxlovid reduced the risk of post-acute inpatient death by 42% in immunocompromised patients who were admitted to hospital with COVID-19. The second study emphasised that the effectiveness of Paxlovid can be modified by COVID-19 vaccination status, suggesting patients who were not fully vaccinated and were not prescribed Paxlovid faced a compounded increase in risk.

The role of Paxlovid in reducing post-acute mortality among immunocompromised COVID-19 patients
Immunocompromised individuals are often underrepresented in randomised controlled COVID-19 trials and are typically excluded from assessments of antiviral interventions. To address this gap, CUHK researchers used real-world data to conduct a study, published in The Lancet Rheumatology, examining the effects of Paxlovid in this high-risk population.
The research team analysed 39,923 eligible patients aged 18 and above in Hong Kong between March 2022 and November 2023, using real-world COVID-19 surveillance data obtained from the Hong Kong Hospital Authority and Department of Health. Among them, 846 (38.2%) of 2,217 patients who were immunocompromised and 14,586 (38.7%) of 37,706 patients who were immunocompetent were prescribed Paxlovid within five days of symptom onset. The study compared outcomes between groups based on immune status (immunocompromised or immunocompetent) and Paxlovid use.
The key findings are as follows:
- Reduced mortality: immunocompromised patients prescribed Paxlovid had a 42% lower risk of post-acute inpatient death compared to those who did not receive the antiviral.
- Respiratory benefits: Paxlovid also reduced the risk of post-acute hospitalisation due to acute respiratory distress syndrome by 57% among treated immunocompromised patients.
- Immunocompetent comparison: in immunocompetent patients, Paxlovid demonstrated even greater reductions in post-acute mortality and all-cause rehospitalisation.
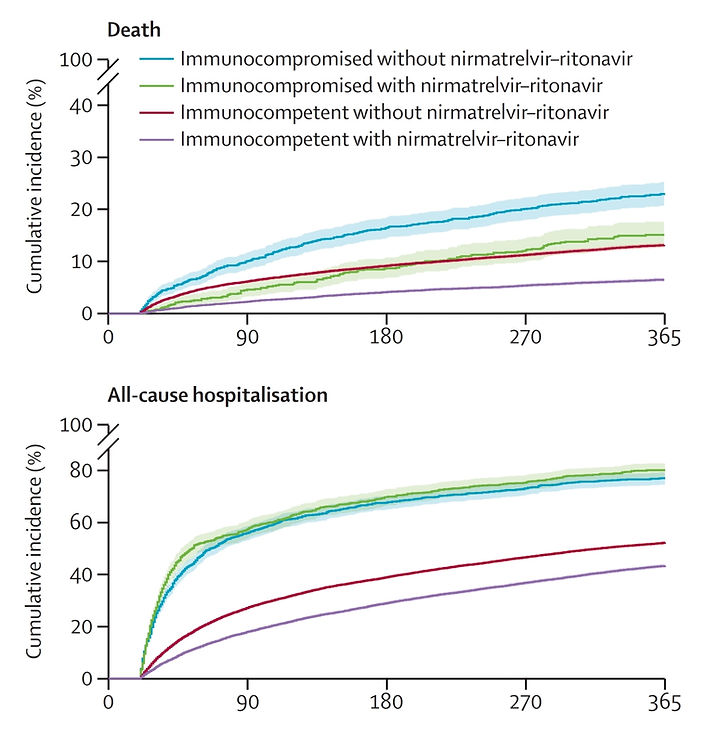
Study results show immunocompromised patients prescribed Paxlovid had a 42% lower risk of post-acute inpatient death compared to those who did not receive the antiviral. Meanwhile, the antiviral demonstrated effectiveness in the reduction of all-cause rehospitalisation in immunocompetent patients.
Professor Marc Chong Ka-chun, corresponding author of the study and Assistant Professor at The Jockey Club School of Public Health and Primary Care at CU Medicine, said: “This study highlights the significant role of Paxlovid in mitigating the long-term risks of COVID-19 for immunocompromised patients, which supports the recommendation that this population use Paxlovid. Nevertheless, our findings also suggest that Paxlovid was less effective for post-acute hospitalisation outcomes in immunocompromised patients than immunocompetent patients. Considering this, longer courses of Paxlovid or combination therapies might be necessary to achieve better long-term results for immunocompromised patients with COVID-19.”
Vaccination amplified the protective effects of Paxlovid
The other study, published in Emerging Microbes & Infections, explored how COVID-19 vaccination interacts with Paxlovid to enhance outcomes. While prior studies have explored antiviral-vaccine interactions through subgroup analyses, this is the first comprehensive study specifically designed to examine how Paxlovid interacts with full vaccination status and its impact on post-acute outcomes.
This research, including over 50,000 hospitalised COVID-19 patients, categorised into four exposure groups based on their use of Paxlovid and vaccination status, revealed that vaccination significantly amplifies the drug’s effectiveness in reducing post-acute rehospitalisation among COVID-19 patients.
The study has found that:
- Synergistic effects: fully vaccinated patients prescribed Paxlovid experienced the lowest rates of post-acute mortality and rehospitalisation compared to other groups.
- Additive interactions: vaccination amplified the protective effects of Paxlovid, particularly in reducing the risk of post-acute rehospitalisation, while the interaction effect on post-acute mortality was marginally significant.
Professor Yeoh Eng-kiong, corresponding author of the study and Director at the Centre for Health Systems and Policy Research at CU Medicine’s The Jockey Club School of Public Health and Primary Care, said, “Our findings highlight the crucial role of integrating vaccination with antiviral treatments like Paxlovid. The synergy between the two interventions underscores the need for comprehensive strategies to manage both acute and post-acute COVID-19 conditions.”
The studies were supported by the Health and Medical Research Fund, Research Grants Council Theme-based Research Scheme and Research Grants Council Collaborative Research Fund. The full studies can be accessed at:
https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913(24)00224-8/fulltext?rss=yes
https://www.tandfonline.com/doi/full/10.1080/22221751.2024.2421397