Tracheal cancer is a relatively rare malignancy with a high mortality rate. Though smoking has been confirmed as one of the factors, the exact cause of the cancer is not yet fully understood. The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) conducted a study with the Association of Pacific Rim Universities (APRU) to reveal the 10-year global epidemiology of this rarely seen cancer. The findings showed association with factors such as Human Development Index (HDI), Gross Domestic Product (GDP) per capita, genetics and lifestyle. The global incidence of tracheal cancer had been in decline but the incidence rates of females and the younger population in certain regions edged up.
Researchers recommend continued focus on high-risk groups and strengthening health education. Details of the study have been published in the prestigious international medical journal Molecular Cancer.

Research and treatment of tracheal cancer are limited compared to bronchial and lung cancers
The trachea, connecting the larynx with the bronchi, is part of the respiratory system. The bronchi then carry inhaled air to the lungs. Common symptoms of tracheal cancer include chronic coughs, blood in mucus during coughing, difficulty in swallowing and breathing, hoarseness, gasping and wheezing. As tracheal cancer is often grouped with bronchial and lung cancers, given that it represents less than 1% of all malignant diseases, there is a lack of up-to-date research data in the medical field. Patients often present advanced stage at primary diagnosis and treatments available are also limited, with a 5-year survival rate of less than 30%.
Incidence rates are higher in the European and Mediterranean regions
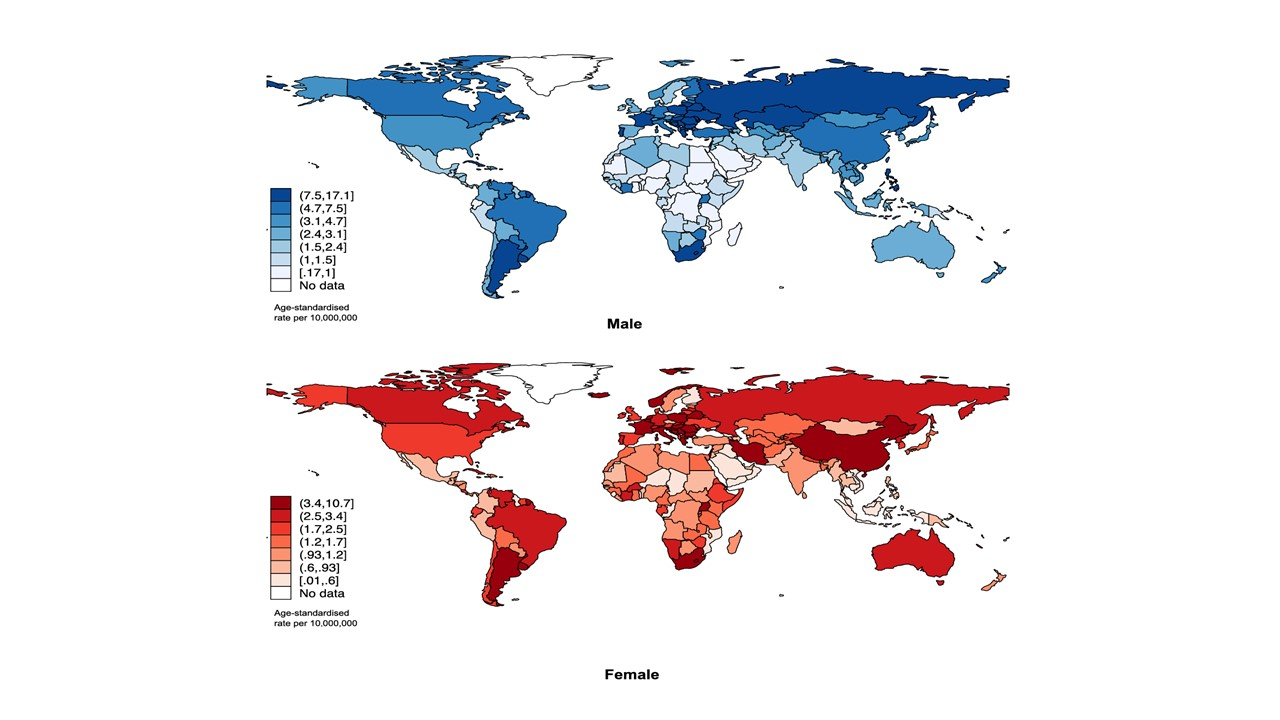
The CU Medicine research team calculated and analysed the incidence of the cancer and the prevalence of each risk factor by collecting 10 years of data from databases such as the Global Cancer Observatory, Cancer Incidence in Five Continents and Global Burden of Disease. As estimated by the researchers, there were 3,474 tracheal cancer cases globally, with an age-standardised rate (ASR) of 2.9 per 10 million people in 2022. By age and gender, higher incidence of trachea cancer was found among older people aged from 50 to 74 years old and among males when compared with females. Central and Eastern Europe were the subregions with the highest ASR (see Table 1 for details). On a country level, the ASR of Hungary was notably higher than other countries (see Table 2 for details).
Table 1: Top three regions with the highest ASR of tracheal cancer incidence
| Top three locations with the highest incidence | ASR of incidence (per 10,000,000) |
| Central and Eastern Europe | 9 |
| Western Europe | 5 |
| Southern Europe | 5 |
Table 2: Top three countries with the highest ASR of tracheal cancer incidence
| Top three locations with the highest incidence | ASR of incidence (per 10,000,000) |
| Hungary | 13 |
| Guadeloupe, France | 11 |
| Croatia | 10 |
Dr Jason Huang Junjie, the first author of the study and Assistant Professor from The Jockey Club School of Public Health and Primary Care at CU Medicine, stated: ‘‘Globally, for unknown reasons, the incidence of tracheal cancer was higher in the European and Mediterranean regions, probably due to genetics and geographical environment. This finding reminds public health policymakers to focus on these locations, strengthen preventive measures for tracheal cancer and further explore the ties between genetic and environmental factors.”
Urban development affects the incidence of tracheal cancer
The tracheal cancer incidence ratio is highly associated with multiple factors, notably HDI and GDP per capita. This trend probably reflected more complex lifestyle and environmental factors, with the prevalence of smoking and alcoholism being critical risk factors that are not only detrimental to the respiratory system but also harmful to overall health. In addition, unhealthy eating habits and an inactive lifestyle could also be associated with a higher risk of tracheal cancer, particularly obesity, which would probably increase the susceptibility to cancers by affecting the immune system and endocrine functions. Other health conditions such as hypertension, diabetes and lipid abnormalities were also associated with a higher risk of tracheal cancer.
Dr Claire Zhong Chenwen, the co-corresponding author of the study and Research Assistant Professorfrom The Jockey Club School of Public Health and Primary Care at CU Medicine, commented: ‘‘The study revealed the relationship between tracheal cancer and factors such as high HDI, smoking, alcoholism, unhealthy diet and lack of exercise, suggesting the need for early intervention to address these controllable risk factors. Public health policies should focus on strengthening health education, facilitating the promotion of a healthy lifestyle and providing the necessary support and resources to high-risk groups to reduce the incidence of tracheal cancer.’’
Incidence ratios of females and younger population increase in certain regions despite the decline in overall incidence of tracheal cancer
Over the past decade, with stronger health awareness, there has been a decreasing trend in the global incidence of tracheal cancer, particularly among the male population and the elderly while the decline was less evident for the female population and younger individuals (aged 15-49 years old). However, higher incidence was identified in some countries. Among younger individuals, there was significantly higher tracheal cancer incidence in Ireland and Colombia (Average Annual Percentage Change [AAPC]*): 30), followed by India and Malta (AAPC: 15). In the female population, Colombia (AAPC: 19), Norway (AAPC: 16) and Kuwait (AAPC: 15) were found to see higher incidence ratios of tracheal cancer.
Researchers see the need of further research of the cancer in countries such as China. The average global incidence rate was 2.9 while China had an incidence up to 4.7, which was higher than countries in East Asia such as Korea, Japan and Mongolia. While there has been a relatively stable incidence rate among females and a potential uptick among the elderly in China, more in-depth research is required to better understand the underlying reasons.
Professor Martin Wong Chi-sang, the senior corresponding author of the study and Professor of The Jockey Club School of Public Health and Primary Care at CU Medicine, added: ‘‘Despite the declining incidence of tracheal cancer as a whole, the rising incidence among younger individuals and females in certain locations has sounded an alarm to us that the health conditions of these groups should remain a focus for us. The rising tracheal cancer incidence may be related to changes in lifestyle. Hence, health education and intervention measures targeting these groups should be reinforced to prevent the incidence from escalating further in the future.’’
* AAPC is a measure of the overall changes in the cancer incidence for a specific period. For example, if the cancer incidence AAPC of a country is 5 for the past 10 years, it means the cancer incidence in that country increased 5% on average each year over the 10-year period.
About the joint study with APRU
This paper is a collaboration with Professor Mellissa Withers, Director of the APRU Global Health Programme; Keck School of Medicine, University of Southern California. The APRU (https://apru.org/) was established in Los Angeles in 1997 by the presidents of UCLA, Berkeley, Caltech and the University of Southern California. It now has a membership of 61 leading research universities from around the Pacific Rim. CUHK is an important member of the APRU, with Professor Martin Wong Chi-sang currently serving as its expert adviser, and Dr. Jason Huang Junjie and Dr Claire Zhong Chenwen